During pregnancy it is important for both you and your baby that you eat well. Your choices of what to eat and drink at this time can affect your health and the health of your baby for many years to come.
There is only a small increase in the amount of food you need to eat while you are pregnant.
However, you do need more of certain nutrients, so it is very important that you make good choices for a nutritious diet.
Folate is needed for the growth and development of your baby. It is especially important in the month before you fall pregnant and the first trimester (three months) of pregnancy.
A good intake of folate reduces the risks of your baby being born with some abnormalities such as spina bifida (a disorder where the baby’s spinal cord does not form properly).
Dietary sources high in folate include:
Women planning a pregnancy and in the early stages of pregnancy should eat a variety of folate-containing foods. You should also take a folic acid supplement of 400 micrograms per day at least one month before, and three months after, you become pregnant.
You need more iron during pregnancy. If you do not have enough iron, you may develop anaemia.
Good sources of iron include:
If you are low in iron, your doctor or midwife may suggest taking an iron supplement (tablet or liquid).
You can help your body get iron from the food you eat or drink by:
Pregnant women need 27 mg iron each day. Pregnant women should not eat more than 45 mg iron each day.
Adequate iodine in pregnancy is essential for your baby’s growth and brain development.
Iodine is important for your baby’s development in the womb.
Good food sources of iodine include:
Pregnant women should take a supplement containing 150 micrograms of iodine each day.
A multivitamin during pregnancy is not necessary unless you do not have a balanced diet. Compare what you are eating with the following food group table.
Remember, a folic acid supplement is important during the first trimester of pregnancy, and iodine is essential during pregnancy (and breastfeeding). You may also need to take an iron supplement if your iron levels are low.
You may choose to get these nutrients from individual tablets or from a multivitamin.
Always check with your doctor or midwife before taking any supplements, as an excessive intake of these can be harmful and reduce the absorption of other nutrients.
More information: Queensland Health Nutritional Education Materials Online (NEMO)
Food group | Serves per day (for 19-50 year olds) | 1 serve equals |
|---|---|---|
Vegetables and legumes/beans | 5 | ½ cup cooked green or orange vegetables (e.g. broccoli, carrot, pumpkin or spinach) ½ cup cooked, dried or canned beans, chickpeas or lentils (no added salt) 1 cup raw leafy green vegetables ½ medium potato, or other starchy vegetable (sweet potato, taro, or cassava) ½ cup sweet corn 75g other vegetables (e.g. 1 small-medium tomato) |
Fruit | 2 | 1 piece medium sized fruit (e.g. apple, banana, orange, pear) 2 pieces smaller fruit (e.g. apricot, kiwi fruit, plums) 1 cup diced, cooked or canned fruit ½ cup 100% juice 30g dried fruit (e.g. 1½ tbsp sultanas, 4 dried apricot halves) |
Grain (cereal) foods - mostly wholegrain | 8½ | 1 slice of bread ½ medium bread roll or flat bread ½ cup cooked rice, pasta, noodles, polenta, quinoa, barley, porridge, buckwheat, semolina, cornmeal ⅔ cup breakfast cereal flakes ¼ cup muesli 3 crisp breads 1 crumpet or 1 small English muffin or scone |
Lean meat and poultry, fish, eggs, nuts and seeds, and legumes/beans | 3½ | 65g cooked lean red meats (e.g. beef, lamb, pork, venison or kangaroo) or ½ cup lean mince, 2 small chops, 2 slices roast meat 80g cooked poultry (e.g. chicken, turkey) 100g cooked fish fillet or 1 small can fish, no added salt, not in brine 2 large eggs (120g) 1 cup (170g) cooked dried beans, lentils, chickpeas, split peas, canned beans 170g tofu ⅓ cup (30g) unsalted nuts, seeds or paste, no added salt |
Milk, yogurt, cheese and/or alternatives - mostly reduced fat | 2½ | 1 cup (250ml) milk 40 g (2 slices) hard cheese (e.g. cheddar) 120g ricotta cheese 200g yoghurt |
The weight you should aim to gain will depend on what your body mass index (BMI) was before you became pregnant. Use this tool to calculate your BMI.
Your BMI is the number used to work out your recommended amount of weight gain.
Pre-pregnancy BMI | Recommended total gain | Weekly guide in 2nd and 3rd trimester |
Less than 18.5 kg/m² | 12½ to 18kg | 1/2 kg per week |
18.5 to 24.9 kg/m² | 11½ to 16kg | 400g per week |
25 to 29.9 kg/m² | 7 to 11½ kg | Less than 300g per week |
Above 30 kg/m² | 5 to 9kg | Less than 300g per week |
You may find it easier to follow a pregnancy weight gain chart. The charts are divided in two groups:
More information: How much weight should I gain while pregnant.
Listeria is a bacteria found in some foods, which can cause an infection called listeriosis. If passed on to your unborn baby it can cause premature birth, miscarriage or damage. Throughout your pregnancy, it is important to avoid foods that have a high risk of containing listeria.
Foods that might contain Listeria and should be avoided include:
Fish is a safe and important part of a healthy diet. It is an excellent source of protein, low in saturated fat, high in omega 3 fish oils and a good source of iodine.
However, some types of fish should be restricted as they may contain higher levels of mercury.
Recommendations for pregnant women
(1 serve = 150g)
1 serve per fortnight of shark (flake) or billfish (swordfish/broadbill and marlin) and NO other fish that fortnight
or
1 serve per week of Orange Roughy (Deep Sea Perch) or catfish and NO other fish that week
or
2–3 serves per week of any other fish and seafood not listed above.
Do not eat raw or undercooked eggs. Eggs must be cooked through so that both the white and yolk are hard.
Here are some tips for keeping your food safe:
More information on healthy eating during pregnancy, including fact sheets and resources suitable for Aboriginal, Torres Strait Islander, Maori, and Pacific Islander women are available through Queensland Health Nutritional Education Materials Online (NEMO).
It’s great to be active and stay fit while you’re pregnant.
Check with your doctor or midwife to make sure there are no health problems to prevent you from exercising.
If there are no problems, try to do 30 minutes of moderate exercise (like walking) on most days of the week.
Regular exercise can help you:
Pregnancy can increase your risk of injury because your joints loosen up to let your body grow and make it easier to give birth.
You can prevent injury in pregnancy by avoiding high impact exercise like jumping up and down, repetitive bouncing movements, and any movements that over-stretch your hip, knee, ankle or elbow joints.
Stop exercising if you experience:
Read more information on pregnancy and exercise.
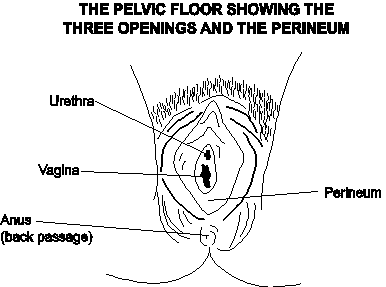
By performing pelvic floor exercises, you can strengthen muscles to help reduce or avoid stress incontinence after pregnancy.
Incontinence is a common but treatable condition – view the video below or visit the Continence Foundation of Australia for more information.
To learn safe exercises, you can download a copy of Pelvic floor health for expectant and new mums from the Continence Foundation of Australia.
This video answers the question about why a woman has an increased risk of leaking urine (urinary incontinence) after childbirth. Find out how to prevent this from happening, how to treat the condition and where to get help.
From about 35 weeks you can start preparing for your labour and birth with perineal massage.
Research has shown that massaging the perineum during late pregnancy may encourage elasticity and reduce the risk of tearing during childbirth.
The perineum is the area between the vaginal opening and anus. Some women choose to use perineal massage as a way of (hopefully) reducing their risk of perineal trauma during childbirth.
You can start massage from about 35 weeks and perform no more than three times per fortnight.
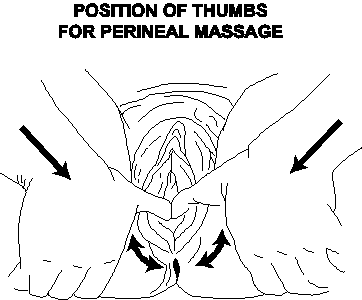
Ask your doctor or midwife for more information.
Not all medicines are safe during pregnancy and breastfeeding.
This includes medicines that are prescribed, natural supplements, or over the counter from the pharmacy or supermarket.
Make sure you tell your doctor or midwife, and pharmacist, about all the medicines you are taking – especially if you:
More information: Queensland Clinical Guidelines – Using drugs in pregnancy
The safest choice for your baby is to not drink any alcohol.
The risk of damage to your baby increases the more you drink, and binge drinking is especially harmful.
There is no safe amount of alcohol to drink when you’re pregnant.
If you drank small amounts of alcohol before you knew you were pregnant, be reassured that the risk of harm to your baby is low.
More information: The National Organisation for Fetal Alcohol Syndrome. Alcohol and Pregnancy
Stop smoking during pregnancy and you and your baby will immediately feel the benefits.
Toxic chemicals are absorbed into your bloodstream and passed on to your baby through the umbilical cord. If you are unable to stop smoking, cut down as much as you can.
For advice and support visit Quit HQ or call Quitline on 13 78 48.
More information: Pregnancy Birth and Baby - Smoking and pregnancy
When you feel the urge to smoke:

More information: Coping with quitting and staying smoke- and vape-free
Immunisation is a simple and effective way to protect yourself and your baby from certain infections.
During pregnancy, it is recommended that you have the following vaccinations.
Influenza can cause serious illness and being pregnant increases the risk of influenza complications, especially with the H1N1 influenza virus. Influenza vaccine is safe and can be administered before, during or after pregnancy.
Whooping cough can cause serious illness and even death in babies less than six months old. It is now recommended that all pregnant women receive a pertussis (whooping cough) vaccination during their third trimester (ideally at 28 weeks) of every pregnancy.
Check with your doctor whether you have immunity against measles, mumps, rubella, chickenpox – as well as influenza and whooping cough.
More information:
Coronavirus (COVID-19) is a new virus and we are still learning how it may affect you and your baby.
There is currently no cure, treatment or vaccine to prevent COVID-19. To reduce your chance of getting the virus, follow prevention measures
Regularly check the COVID-19 pregnant and breastfeeding women page for updated information.
Read about the common viral infection cytomegalovirus (CMV).
It is important to wear gloves when gardening and wash hands afterwards.
Cats can be a source of Toxoplasmosis – a serious infection that can cause defects or death in your baby. It is important to avoid contact with cats and use gloves when handling cat litter.
Looking after yourself and your baby, 23 Mar 2023, [https://oss-uat.clients.squiz.net/health/children/pregnancy/antenatal-information/looking-after-yourself-and-your-baby]
This document is uncontrolled when printed. Before using the information in this document you should verify the current content on https://oss-uat.clients.squiz.net/health/children/pregnancy/antenatal-information/looking-after-yourself-and-your-baby.