A normal, problem-free labour is every pregnant woman's wish, however medical interventions are sometimes needed to help with the birth of a baby.
Assisted vaginal birth accounts for around 11% of births in Australia. Reasons include:
-
Assisted birth – vacuum birth
Vacuum birth
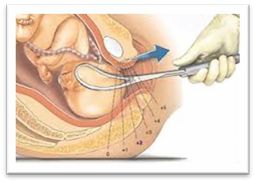
This is the more common technique used for assisted deliveries. The vacuum cup is made of plastic and is attached to a suction device. A doctor inserts the cup into the vagina and creates a vacuum against the baby’s head. This helps the doctor to gently pull the baby out as you push.
What do I need to know?
- you may need an episiotomy
- if vacuum birth fails, a caesarean birth might be needed
- serious baby injuries after a vacuum birth are rare but can include bleeding under the scalp called a cephalhematoma
- it may cause a raised bruise on the baby’s head, but this soon fades
- minor scalp wounds from the pressure of the cup can occur.
More information: The Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG) – Assisted birth
-
Assisted birth – forceps birth
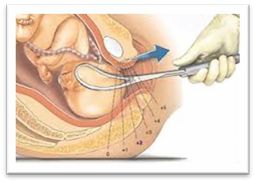
A doctor applies forceps, an instrument shaped like a pair of large spoons or ‘salad tongs’, to the baby's head to help guide the baby out of the birth canal. This is done during a contraction while you push.
Forceps birth and baby
What do I need to know?
- you may need an episiotomy
- if forceps birth fails, a caesarean birth might be needed.
Your baby may experience:
- minor marks on the face which are temporary
- minor facial injuries due to the pressure of the forceps
- temporary weakness in the facial muscles (facial palsy)
- minor external eye trauma.
Serious baby injuries after a forceps birth are rare but could include:
- skull fracture
- bleeding within the skull
- seizures.
More information:

-
Caesarean birth
Around one in four Australian babies is birthed by caesarean section. A caesarean section is usually performed under regional (spinal or epidural) anaesthesia. However, sometimes general anaesthesia is required.
A caesarean section is a major surgical operation in which your baby is born through a cut in your abdomen and uterus.
Elective caesarean births are planned in advance because of existing problems with your pregnancy, or if you have had a previous caesarean.
Emergency caesarean births - usually the decision to perform an emergency caesarean is made during the course of labour. An emergency caesarean birth is recommended for the following reasons:
- there is concern for your baby’s wellbeing
- there is concern for your wellbeing
- there is a life-threatening emergency for you or your baby.
More information: Pregnancy, Birth and Baby – Caesarean
Elective caesarean birth
A planned or elective caesarean birth is required when there is a medical need for the operation. Medical reasons for having a planned caesarean birth include, but are not limited to:
- severe pre-eclampsia
- multiple births
- position of the baby – your baby may be in an abnormal position inside the uterus, making vaginal birth difficult
- placenta praevia – this is when the placenta blocks the exit to the uterus
- infection – if you have an active viral infection, such as genital herpes
- you have a medical condition – for example, a heart problem
- restricted growth of the baby
- previous caesarean birth.
More information:
Emergency caesarean birth
In an emergency, there may not be enough time to discuss the options of a caesarean birth. If vaginal birth poses significant risks to you or your baby’s health, a caesarean birth may be the safest option.
Reasons for needing an emergency caesarean birth include:
- Your baby cannot tolerate uterine contractions and gets distressed
- your labour is not progressing - despite your best efforts - causing distress to you and your baby
- your labour has been induced, but the methods used are failing to produce effective contractions
- you have vaginal bleeding during your labour
- an emergency where baby needs to be born very quickly and vaginal birth is not possible.
More information: Pregnancy, Birth and Baby – Emergency caesarean
-
What can I expect for a caesarean birth?
Before your surgery (if elective):
- you will need to meet an anaesthetist. This may be in a ‘pre-admission’ appointment at the hospital to talk about your anaesthetic for surgery
- you may be asked to take an antacid tablet, at home, the night before surgery
- you will need to fast from midnight, the night before the morning ‘list’ for elective surgery (or at another time specified)
- a small shave of the top part of the pubic area may be recommended, where the wound dressing will be applied after the surgery
- you will need to remove all jewellery, piercings and nail polish prior to surgery (toe nail polish may be acceptable but not fingernails).
On the day of your surgery (elective or emergency):
- you will be placed in a hospital gown, compression stockings and theatre cap
- a cannula will be inserted into your hand/arm (to give you intravenous medications)
- you will be given an epidural, if you have not already had one during labour
- once the epidural is working well, you will have a urinary catheter inserted into your bladder, as you will be unable to go to the toilet with an epidural in place
- you are usually in the operating theatre for an hour or more
- unless you are having a general anaesthetic, your partner can be with you in the operating theatre
- your partner will need to wear closed-in shoes, for workplace health and safety reasons
- you will have a midwife stay with you and look after you and your baby in theatre and afterwards in the recovery area
- unless you have had a general anaesthetic, skin to skin contact with your baby will occur very soon after birth
- the midwife will help you with feeding your baby.
Where will my baby go?
After your caesarean birth
- if you and your baby are both well, your baby will go with you to the postnatal ward and ‘room-in’
- if your baby is unwell, or needs to be monitored more closely, he/she may need to go to the Special Care Unit or Neonatal (newborn) Intensive Care Unit. Your partner may go with your baby until you are able to join them
- if your baby is unable to have skin to skin contact or breastfeed, you will be encouraged to express breast milk for your baby. Your midwife will assist you with this.
Caesarean birth recovery
How long will I be in hospital?
After your caesarean birth, you will stay in hospital for about three to five days.
A caesarean birth is major surgery, so your physical recovery is important. This is also a great time to get to know your new baby, with the support of hospital midwives and doctors.
Vaginal birth after caesarean (VBAC) is possible. After a previous caesarean birth, around 60–80% of women who attempt labour will have a vaginal birth.
More information:
-
Risks of caesarean birth
Complications of a caesarean birth are rare but can include:
- Increased likelihood of blood loss. Depending on the degree of bleeding, some women may require a blood transfusion and/or hysterectomy (this is very rare).
- Risk of complications associated with having surgery, such as blood clots, scalpel cuts to the bladder or bowel (this is rare).
- Risk of a wound infection.
- Slower recovery time.
- Increased likelihood of complications in future pregnancies. For example, the placenta being low lying (placenta previa) or growing into the scar on the uterus (placenta accreta) which can lead to severe bleeding or further caesarean birth(s).
- Risk of baby having breathing problems and requiring admission to the Neonatal Intensive Care Unit or Special Care Nursery.
- Risk of scalpel cuts to the baby.
- Increased likelihood of the baby having feeding problems.
More information: Queensland Government – Caesarean Section Consent form
This document is uncontrolled when printed. Before using the information in this document you should verify the current content on https://oss-uat.clients.squiz.net/health/children/pregnancy/antenatal-information/assisted-birth-and-caesarean-birth.