Breastfeeding Guide
-
Breastfeeding 101
Why breast milk?
Perfect food
Breastfeeding is the natural, biological way of providing babies with nutrients required for healthy growth and development.
Better for mum, better for baby
Breastfeeding helps with mother and baby emotional attachment and is better for both short and long term health.
Environmentally friendly
Breast milk has no waste products, so it is better for the environment.
Risks of not breastfeeding
For mothers
Higher risk of:
- ovarian cancer
- breast cancer
- type 2 diabetes.
More expensive:
- cost of formula
- cost of healthcare for a sick baby.
For babies
Higher risk of:
- gastrointestinal infections
- chest infections
- ear infections
- childhood leukaemia
- SIDS (sudden infant death syndrome)
- some long term diseases, for example diabetes
- allergies and milk intolerances.
For the community
- higher healthcare costs
- using up natural resources
- higher waste products in the environment.
Babies know how to breastfeed
Babies know when they are hungry and thirsty. Babies know when the milk comes in. Babies know how to breastfeed.
Allowing babies to do what they were born to do, will make for a much smoother transition into this new world; for mother and baby.
More information:
- Queensland Clinical Guidelines parent information – Breastfeeding your baby
- Breastfeeding information in other languages:
- Breastfeeding and postnatal care, Victorian Government
- Breastfeeding your baby, Royal Women's Hospital, Victoria
- Breastfeeding resources in other languages, Australian Breastfeeding Association
- Global Health Media – Breastfeeding videos in other languages
- Queensland Health – Breastfeeding information for Aboriginal & Torres Strait Islander people
What are the recommendations?
The World Health Organization and the National Health and Medical Research Council (NHMRC) recommend you breastfeed your baby exclusively for the first six months. Breast milk is all the food and drink that a baby needs.
The Australian Dietary Guidelines (NHMRC) recommends:
- breastfeeding as the best method of feeding full-term babies
- exclusive breastfeeding for around six months of life
- breastfeeding continues beyond six months while appropriate solid foods are introduced
- along with solids, women are advised to continue breastfeeding until 12 months of age, for as long as the mother and child decide.
Baby-friendly Hospital Initiative
The Baby-friendly Hospital Initiative (BFHI) was developed by the World Health Organisation and UNICEF in 1991. It is a worldwide program aiming to create a healthcare environment that supports mothers and babies to have the best start in life.
Queensland Health is proud to support the BFHI. We promote breastfeeding as the optimal way to feed your baby; however we also respect how you choose to feed your baby.
-
In pregnancy – planning for breastfeeding
Think about what is important for you.
It is never too early to read, learn and talk about breastfeeding.
Most people have a view about breastfeeding before having their baby. What have you heard from friends, television, or in the community?
Pregnancy – breast changes
Learning about the changes in your breasts during pregnancy may give you a better understanding of your body’s ability to breastfeed. The good news is, no physical preparation is required!
Most women notice breast changes in pregnancy, however some do not. Your breasts will usually increase in size – as the due date approaches, hormone changes cause your breasts to feel larger and tender. Sometimes, visible veins appear. In the third trimester, some pregnant women begin to leak colostrum from their breasts.
How your body makes milk
Your breasts are filled with milk making glands that are called alveoli. This is where your milk is produced. The milk travels from the alveoli through a series of milk ducts to the nipple openings.
The more often your baby breastfeeds, the more milk your breasts make.
Breastfeeding hormones
When your baby breastfeeds, your brain releases two hormones.
Prolactin is the hormone that causes your breasts to make milk.
Oxytocin helps with your letdown reflex (release of milk). These hormones also increase the level of bonding and comfort you feel during breastfeeding.
What happens during milk let down?
When your baby latches on and begins to breastfeed, the alveoli release milk. This is called the let down or milk ejection reflex. Let down occurs several times during a feed. In the early days, you may not even notice this is happening.
How can I tell if my milk is letting down?
- sensation of warmth or tingling in the breast
- sudden thirst
- milk dripping from the other breast
- ‘after birth’ pains
- changes in the baby’s sucking pattern from quicker sucks to slower deeper sucks.
More information: Australian Breastfeeding Association – Breastfeeding Information
Can all mothers breastfeed?
Most women can breastfeed with the right information, support and practice.
Speak to your midwife, doctor or lactation consultant if any of the following applies to you:
- previous breast surgery
- a medical condition requiring medications
- diabetes
- your current pregnancy is twins (triplets, quads, etc).
More information: Australian Breastfeeding Association
Things to think about while you are pregnant
- Why have you decided to breastfeed your baby?
- What information about breastfeeding do you already have?
- Are family members supportive of your interest in breastfeeding?
- Will someone be at home to help you in the early weeks?
- Do you have any special medical problems that require treatment or medications?
- Have you ever had breast surgery? What was the reason?
- How long do you plan to breastfeed?
- Do you plan to return to work/school/study after your baby is born?
- If you have breastfed other children:
- How long did you breastfeed?
- Why did you stop?
- Did you have any problems?
-
Breastfeeding – the first few days
The first feed
Most babies will attach to the breast for their first feed if placed skin to skin (in contact) with their mother.
Skin to skin contact
This is when your baby is placed directly from birth onto your chest or abdomen. Your newborn’s skin touches your skin. A blanket or towel can be placed over the baby’s back for warmth if required. Providing baby and you are well, skin to skin contact should continue, undisturbed, until the first breastfeed. Routine procedures such as bathing and weighing can wait.
If you can’t have skin to skin right after the birth, this is often due to medical reasons.
Your midwife will support skin to skin contact as soon as possible.
More information: Queensland Clinical Guidelines parent information – Breastfeeding your baby

Most healthy babies will want to feed within the first 90 minutes after birth.
During skin to skin contact, your baby will show feeding signs (cues).
When this happens, position baby close to your breast.
Bonding and rooming in
After your baby is born, you will both be in the same room – you will be able to see signs that your baby is hungry, uncomfortable or needs to be cuddled.
Benefits of rooming in:
- babies cry less and are easier to calm
- mums get more rest
- you can respond to baby's early feeding cues and feed on demand
- you will make more breast milk when you feed your baby often.
The first few days
Newborn feeding behaviour
Birth to two hours
Baby is usually awake and alert (best time to feed).
The first 24 hours
Two to 20 hours after birth, baby will have light and deep sleep (may not want to feed often).
After 20 hours
Baby will have sleep and awake behaviour (and may want to feed often).
Day two to three
Your baby may seem unsettled on day two or three while your colostrum changes to mature milk. Increased breastfeeding is often all that is needed.
More information: NHS – Breastfeeding: the first few days
-
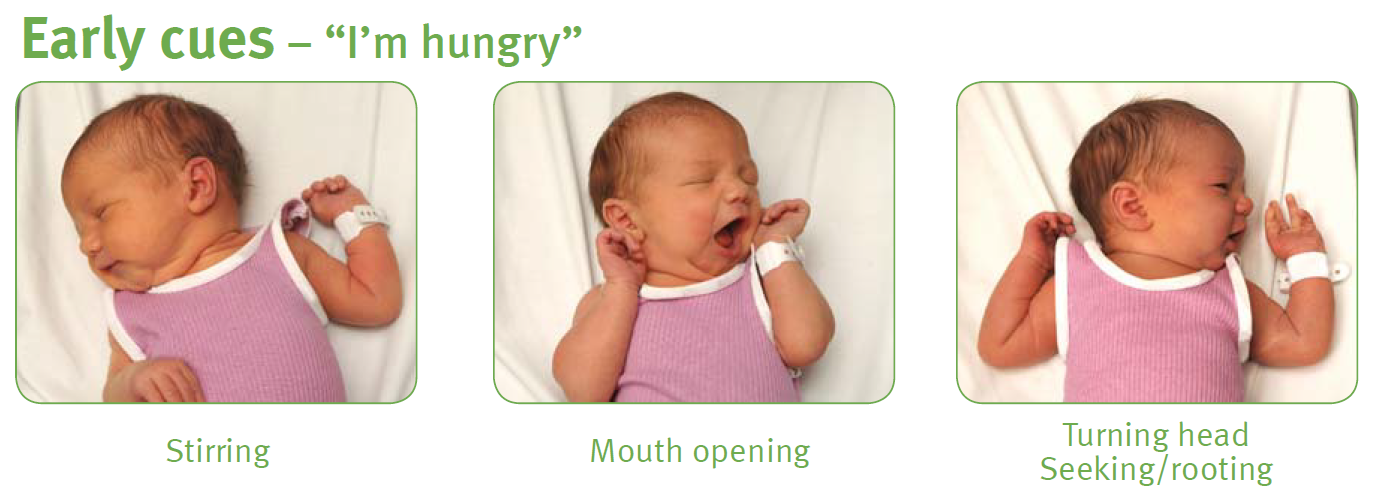
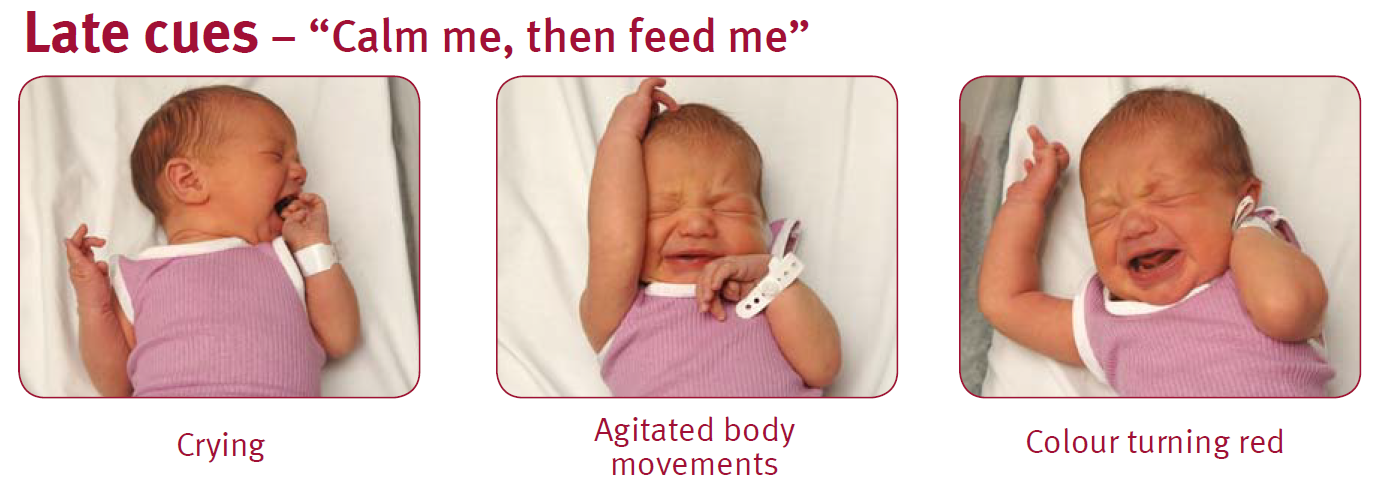
Signs of hunger
Mothers can follow their baby's lead in how often to breastfeed.
Rather than watching the clock, watch for cues that your baby is hungry such as the rooting reflex, chewing/sucking on hands or fingers.
Early feeding cues (signs) are the best time to feed!
Early cues: “I’m hungry” (stirring, mouth opening, turning head and seeking/rooting).
Mid-cues: “I’m really hungry” (stretching, increasing physical movement, hand to mouth).
Late cues: “Calm me, then feed me” (crying, agitated body movements, colour turning red).
-
Breastfeeding – the early weeks
How your milk changes
The first milk is called colostrum. This special milk is yellow in colour, thick and sticky. It may be low in volume but it is high in concentrated nutrition for your newborn.
Colostrum has a laxative effect on baby, helping him or her pass the early stools and helping to prevent jaundice.
The more you feed your baby, the more milk you will make (supply = demand).
Days after birth
Type of milk
How it looks
Birth to day 2 or 3
Colostrum
Thick, yellow in colour, small amount
Days 3 to 5
Transitional milk
Mixture of colostrum and mature milk more plentiful
Days 5 to 7
Mature milk begins
Thinner, whitish, plentiful
When does milk ‘come in’?
You may find that your breasts become larger and feel heavy, warmer and uncomfortable when your milk ‘comes in’; usually about two to four days after your baby is born.
Your milk will then increase in volume and will generally begin to appear thinner and whiter in colour.
How often will baby feed?
Whenever baby is hungry!
Healthy, full-term newborns should breastfeed eight to 12 times in each 24 hour period. Many mothers are surprised at how quickly and easily human milk is digested, often within 90 minutes of the last feed.
Many babies do what is called 'cluster feeding’, spacing feeds closer together at certain times of the day (usually during the evening). This is normal. As babies grow and their stomachs become larger, they begin to go longer between feeds and develop more regular feeding patterns.
How long does a feed take?
Your baby will determine this.
A typical feed might last about 20–30 minutes. In the beginning, it could take up to an hour.
It is important that you allow the baby to feed for as long as the baby wants on one side.
Do not time the feed or swap sides unless the baby seems to have finished one side. This will ensure that your baby feeds well and helps with your breast milk supply.
If the baby takes only one breast, remember to offer the other breast at the next feed.
When your baby has had enough, they will stop sucking and come off the breast or simply fall asleep. If you notice that baby's jaw isn't moving anymore, you can detach baby. Your breasts keep making milk.
Remember, supply = demand.
How to tell if your baby is getting enough milk
A common concern to breastfeeding mothers is how to tell whether their baby is getting enough milk.
Your baby will tell you by:
- being content between most feeds
- having six to eight wet nappies a day, by seven days of age
- their poo changing in colour, from black meconium stool to soft yellow by seven days of age
- starting to put on weight. Many babies may lose up to 7% of their birth weight during their first days of life. Babies usually regain the weight by two weeks of age.
Seek advice from a healthcare professional if you have concerns.
Age
Feeds per day
Wet nappies
Dirty nappies
Day 1
3–8
1
1
Black, tarry and sticky
Day 2
5–10
2–3, may contain urates.
What are urates? Crystals present in strong urine that stain a nappy reddish-orange.
1–2
Greenish–black, softening
Day 3
5–10
3–4 paler, but may be concentrated and contain urates.
3–4
Greenish–yellow, soft
Day 4
5–-10
4–6 pale, no urates.
4 large or 10 small
Yellow and/or seedy, soft/liquid
Day 5
8–12
More than 6 pale nappies.
4 large or 10 small
Yellow and/or seedy, soft/liquid
-
Positioning and attachment
The key to successful breastfeeding is comfortable positioning and good attachment.
Make sure your baby is well attached to the breast. If your baby is only attached to the nipple, breastfeeding will be painful.
If your baby is well-attached to your breast, you are less likely to experience breastfeeding problems like cracked nipples, and your baby will get the most amount of milk from your breast.
Find a comfortable place where you can sit and relax. Have everything you might need close to hand – e.g. phone, glass of water. Breastfeeding may take some time.
Positioning and attachment
This webpage is currently being reviewed and some outdated content has been removed. Please refer to Raising Children Breastfeeding videos and Raising Children Breastfeeding positions in pictures in the interim.
Some tips which may help:
- Make sure you are comfortable and well supported. Lean back rather than sit upright. Place your baby on your bare chest between your breasts, facing you. Gravity will help keep your baby in position.
- When calm, your baby will begin to follow their instincts. Your baby will start to move towards one breast. Support your baby behind their shoulders and under their bottom (avoid holding their head). Let your baby move towards your nipple – they know where to go!
- Your baby will most likely position themselves on an angle, with mouth near your nipple and feet supported by your thigh or lap.
- When your baby is just below your nipple, they will dig their chin into your breast, reach up with an open mouth and attach to the breast.
- When your baby is feeding well, they will suck deeply and regularly (sometimes with short pauses), and you’ll hear swallowing.
More information: Raising Children Network – Breastfeeding positions: in pictures
-
Signs of an effective attachment
How to tell if your baby is attached:
- you are comfortable
- baby looks comfortable, relaxed and not tense, frowning or wriggling
- baby’s mouth is open wide against the breast with nipple and breast in mouth
- baby’s chin is touching the breast
- cheeks not sucked in
- baby has deep jaw movement with drinking
- swallowing can be seen and possibly heard once the milk “lets down”
- after feeding, nipples may appear slightly longer but are not flattened, white or pinched.
Video: Raising Children Network – Breastfeeding: getting a good attachment
How to tell if your baby is not attached
Your baby is not attached if:
- baby’s mouth is not open wide
- baby’s lips are curled inwards
- baby has only the nipple or a small amount of breast in the mouth
- you hear a clicking sound when baby is sucking
- you do not hear or see swallowing
- you feel pain when breastfeeding.
Breaking the attachment
Avoid pulling your baby away from your breast. Instead, break the attachment by inserting your little finger into the corner of your baby’s mouth, between the gums, and gently remove your baby from the breast.


-
Breastfeeding positions
Front hold or cradle

Underarm or football hold

Side lying

Video: Raising Children Network – How to breastfeed: breastfeeding positions
More information: Australian Breastfeeding Association – Attachment to the breast
-
Common breastfeeding questions and concerns
Newborn jaundice
Why is my baby’s skin yellow?
Jaundice in the first week of life occurs in 60% of healthy newborn infants. It typically occurs between day two to four after birth and is usually cleared by the first week.
Frequent feeding is the best prevention. If a baby appears to be jaundiced, a blood test can determine the level of bilirubin. Treatment, if any, will depend on the level of bilirubin, how the baby is feeding and how old the baby is. Jaundice appears first on the face and head. If the level of bilirubin goes higher, it will appear on the body, and if it goes even higher it will be on the palms of the hands and soles of the feet.
More information: Queensland Clinical Guidelines parent information – Jaundice in newborn babies
Using a dummy
If you’re breastfeeding, it’s a good idea to avoid using a dummy until breastfeeding is established. This is usually when your baby is four to six weeks old.
Using a dummy (also known as a pacifier) when you plan to breastfeed can:
- lead you to miss those early cues that your baby is ready to feed, thus delaying your milk coming in
- decrease the amount of times you feed your baby
- contribute to low breast milk supply and/or engorgement
- be a factor in low weight gain for baby
- increase baby’s risk of ear and thrush infection
- contribute to an earlier return of your fertility.
More information: Queensland Clinical Guidelines parent information – Breastfeeding your baby
Partners: how can I support my partner?
Partners of new mothers play an important role, they can:
- provide emotional support
- help calm a fussy baby
- bring the new mother food and drink while she is breastfeeding
- reassure the mother that breastfeeding is one of the most important things to give your baby the healthiest start to life
- deflect any negative comments from friends or relatives
- tell her she is doing a great job!
More information:
- Raising Children Network – New dads: 10 tips for making a great start to fatherhood
- Raising Children Network – Grandparents and kinship carers
Video: ACT Government Health – Breastfeeding Give it a Go
Healthy nutrition for breastfeeding mothers
Healthy eating is important when you are breastfeeding.
Your body has a greater need for most nutrients; to meet these needs it is important to eat a healthy, well-balanced diet based on a range of healthy foods and plenty of water.
More information: Queensland Health – Nutrition Education Materials Online (NEMO)
Recommendations about smoking, drinking alcohol and caffeine
Smoking is not recommended while breastfeeding.
Smoking can affect the nutrient content of breastmilk and reduce supply. It also increases the risk of SIDS (sudden infant death syndrome).
Avoid exposing baby to tobacco smoke. Don't let anyone smoke near your baby – whether in the house, car or anywhere else your baby spends time.
For advice and support visit QUIT HQ or call Quitline on 13 78 48.
Alcohol
The safest option is to avoid drinking alcohol while breastfeeding.
Caffeine
Breastfeeding mothers can safely consume caffeine, but they should consume less caffeine than non-breastfeeding women, to protect their health and the health of their breastfed baby.
Medications and breastfeeding
If you have an existing medical condition or are taking an over-the-counter or prescribed medication, discuss this with your health professional.
Always discuss alternative/natural and complementary therapies, as they may not be safe during breastfeeding.
Always check with your doctor or pharmacist regarding prescription and over-the-counter medications when you are breastfeeding.
More information: Australian Breastfeeding Association – Common concerns - baby
-
Common breastfeeding issues
Many women experience some difficulties when establishing breastfeeding.
Most are minor and can be overcome by advice, assistance and support.
Your midwife or a lactation consultant will be happy to help.
For advice contact:
- 13 HEALTH (13 43 25 84)
- Australian Breastfeeding Association Breastfeeding Helpline: 1800 mum 2 mum (1800 686 268)
Engorgement
About three days after having a baby, many mothers will experience breast fullness as their milk 'comes in'. Occasionally a mother may need to express a small amount of milk to soften the breast before a feed. This fullness usually only lasts for 24 hours and is different to engorgement.
Signs of engorgement
- breasts full and painful, with swelling down to areola of breast
- baby may be unable to attach to breast because of fullness.
- limiting the time baby feeds at the breast
- using dummies to extend time between breastfeeds
- baby not being properly attached to the breast.
- massage and warm packs to breast prior to the feed
- express a small amount of milk before feeds to make breasts softer for baby to attach
- feed your baby frequently
- apply cold packs on breast between feeds
- avoid wearing a tight bra
- if symptoms continue, or worsen, seek assistance.
What causes engorgement?
- limiting the time baby feeds at the breast
- using dummies to extend time between breastfeeds
- baby not being properly attached to the breast.
How to treat engorgement
- massage and warm packs to breast prior to the feed
- express a small amount of milk before feeds to make breasts softer for baby to attach
- feed your baby frequently
- apply cold packs on breast between feeds
- avoid wearing a tight bra
- if symptoms continue, or worsen, seek assistance.
Concerns with milk supply
Building your milk supply
When it comes to breastfeeding, remember that supply equals demand. The more you feed your baby, the more milk your breasts will make.
Ways to increase or maintain a good milk supply include:
- respond to your baby’s feeding cues both day and night
- avoid giving any extra feeds from bottles – this reduces your baby’s need to suck at your breast and reduces your milk supply
- avoid the use of dummies until breastfeeding is established (four to six weeks)
- express milk in between feeds to increase your supply.
Sore, damaged nipples
Nipples can be sensitive in the beginning, but breastfeeding should not be painful through a whole feed or continue to be painful.
Helpful hints to avoid sore nipples:
- make sure your baby is well attached to the breast, not just to the nipple
- apply small amounts of expressed breast milk on the nipple after feeding and allow to dry
- replace damp breast pads frequently
- try different feeding positions
- if breastfeeding continues to hurt, or there is nipple damage, seek help.
Cracked/bleeding nipples:
- make sure baby is attached well
- apply small amounts of expressed breast milk on the nipple after feeding
- if there is a need to rest breasts, you should express breastmilk to keep up supply.
If your nipples are cracked or bleeding it is recommended that you seek help from a health care provider.
Mastitis
Mastitis is an inflammation and/or infection of the breast tissue.
Mastitis can be caused by:
- a blocked milk duct or nipple damage
- milk oversupply that is ongoing
- baby not being attached well to the breast
- mother’s stress, fatigue or poor nutrition.
Signs of mastitis
- an area on the breast that is red and swollen
- breast feels hot
- skin on breast may look tight, shiny and red
- mother feels very unwell with flu type symptoms and a temperature greater than 38.5oC – if so, seek medical help immediately.
Management of mastitis
- seek treatment from a doctor immediately – antibiotics should be started
- continue to breastfeed or express to avoid complications
- keep feeding on the side that is not infected and also offer the infected breast (the milk from the affected breast is safe for baby)
- get plenty of rest and drink plenty of fluids.
More information:
- Australian Breastfeeding Association – Common concerns - mum
- Queensland Health – Queensland Milk Bank
Next section: Expressing and storing breastmilk
-
Breastfeeding in the first year
Looking after yourself
Practical support
Involve your family and friends who can provide a network of help with babysitting, social activities and ‘time out’ for you.
Personal support
Talk to friends, family and support groups about how you are feeling.
Information support
Seek information from health professionals, books, websites etc. It can be challenging for you to identify what information is based on the latest recommendations, so be wary of the source of information.
Ways to take care of yourself
- sleep when your baby is sleeping
- limit outside activities and visitors in the early weeks
- drink water when you are thirsty and eat healthy foods
- try to get exercise and fresh air every day
- join a breastfeeding or new mother support group
- talk about your feelings with your partner or others
- let family and friends help with chores
- take as much time off work as practically possible.
Family planning
The return of the menstrual cycle is different for every woman.
Even if you are exclusively breastfeeding, you can start ovulating. That means you can get pregnant again without even knowing that it has happened.
Ask your healthcare professional about your family planning options and if they are compatible with breastfeeding.
Work and breastfeeding
The Australian Breastfeeding Association has useful information on breastfeeding and work.
Newborn sleep and settling
Crying is an important means of communication for young babies. Babies always cry for a reason. These include:
- tiredness
- hunger
- pain
- discomfort, such as being wet, too hot or too cold.
Parenting and adjusting to a new baby is rewarding, but it can also bring significant changes and challenges.
If you or your partner are struggling to cope, there is help available. Call and talk to a relative, friend or visit your Child Health Centre, GP, or health professional.
More information:
- Beyond Blue – Pregnancy and new parents or call 1300 22 4636
- Queensland Health – Mental wellbeing during pregnancy
- Perinatal Anxiety and Depression Australia (PANDA) or call 1300 726 306
When will my baby sleep through the night?
Most baby’s wake and feed at night until about six months of age.
There is a large variation of what is ‘normal’. Prolactin (milk making hormone) levels are highest at night, so night feeds are important to ensure adequate stimulation and milk removal from the breast.
Night feeds are important because they:
- provide up to one third of a baby's nutritional needs in a 24 hour period
- help to maintain your breastmilk supply
- can help to prevent engorgement (full and painful breasts)
- can help delay ovulation (return of period)
- can help mothers and babies relax and feel drowsy, due to the hormone cholecystokinin.
-
Important points about breastfeeding
- No formula can ever have the same ingredients as breastmilk.
- Breastmilk has ‘live’ factors in it that protect against illness.
- Breastfed babies are at lower risk of SIDS.
- Starting solids at around six months of age (with no foods or other drinks before this) will make babies less likely to develop illnesses.
- Babies who are given food earlier than six months of age are not any more likely to sleep through the night.
- Breast milk is approximately 87% water. Breastfed babies don’t require any water, even in hot weather, until around six months of age.
- Feeding 8–12 times in a 24-hour period is normal for breastfed babies.
- When babies have growth spurts (fussy days) they seem to feed constantly.
- Mothers are encouraged to eat a healthy, well balanced diet. There are no foods that breastfeeding women should avoid.
- Drinking more fluids or eating certain foods does not change milk supply.
- It is recommended that breastfed babies do not use dummies for the first four to six weeks.
- Substituting a breastfeed with a bottle on a regular basis can reduce your milk supply.
- Seeking breastfeeding advice or support from a health professional is recommended.
More information:
- Queensland Clinical Guidelines parent information – Breastfeeding your baby
- Australian Breastfeeding Association – Breastfeeding Information
- Queensland Health – Babies and Toddlers
- Queensland Health – Breastfeeding
Next section: Expressing breastmilk
Breastfeeding, 23 Mar 2023, [https://oss-uat.clients.squiz.net/health/children/pregnancy/antenatal-information/breastfeeding-101]
This document is uncontrolled when printed. Before using the information in this document you should verify the current content on https://oss-uat.clients.squiz.net/health/children/pregnancy/antenatal-information/breastfeeding-101.